MDMA’s ideal for therapy because it can “rebrand your sense of self.”
Shame and trauma dance a ghostly tango. An ostracised alcoholic is merely the grown-up version of the abused child we clutch our perals over. Or so says child psychiatrist and leading psychedelic researcher Dr Ben Sessa, presenting to Vital students.
“Abused children generate tremendous sympathy,” says Sessa alluding to many high-profile court cases in the UK during lockdown and beyond, “but once the same abused child turns to addiction, they’re written off as a filthy smackhead, or an alcoholic.” Reported child abuse cases rose a staggering 1493% at one point during the C-19 lockdowns.
Dr Sessa has worked as a child psychiatrist since 1997. But not just with under-16s. He’s taken his knowledge of childhood trauma and applied it across the all-too-adult issues it causes later.
“Existing drugs are not treating the base disorder – trauma”
Like alcohol use disorder (AUD) for example.
“I naturally take a very developmental approach to mental disorder,” he says, “I think that every adult psychiatrist should spend some time as a child and adolescent psychiatrist, because we really do grow up to become our parents. And those things that we learned in those early years – ‘Even my parents can’t love me, I’m useless, I’m a failure, I can’t achieve’ – become a blueprint for the rest of our lives.”
Childhood trauma operates on a scale ranging from forced labour and sustained sexual abuse, to simply growing up in a rigid suburban household where neurotic parents act out their frustrations with a shaming communication style featuring ‘too many shoulds’.
“I deliberately lump together childhood trauma, post traumatic stress disorder, complex post traumatic stress disorder, and addictions,” explains Sessa, “it’s very difficult to treat these, and there’s no single approach.”
The trajectory from trauma to addiction draws on John Bowlby’s attachment theory and research from the past decade or more connecting PTSD to substance abuse. Attachment theory suggests that maladaptive adult behaviour is more likely to be caused by issues between a baby and its mother and other environmental factors including poverty. This contradicts established psychoanalytic narrative, which says it’s all about… the oedipus complex, and other aspects of thanatos, the Freudian ‘drive’ to act according to one’s most selfish, basest urges.
Despite being head of The Tavistock Clinic’s child psychology department from the mid-1940s, Bowlby’s ideas were still being rubbished by the establishment in the 1990s.
“If you’ve had an insecure attachment to your parents, you develop these neuro-protective narratives: ‘I’m bad, I can’t achieve, I’m unlovable, the world is dangerous’,” explains sessa, “By the time you’ve been thinking like this for ten, twenty, thirty years you truly believe it. This is why mental disorders become chronic, lifelong unremitting problems. Faced with it, the safest and simplest way of dealing with it is to numb yourself, block out the world with sedating dangerous substances like heroin. And far more dangerous ones… like alcohol.”
Like in the USA, there’s currently no pharmacological prescription for PTSD available in the UK. Nor alcohol use disorder; in the United States only 4% of AUD sufferers are given a medication.
“We have what we call ‘polypharmacy’,” explains Sessa, “If the patient’s depressed, we’ll give them an antidepressant. If they can’t sleep, we’ll give them a hypnotic. If they’re constantly anxious, we’ll give them an anxiolytic. If their mood goes up and down, we’ll give them a mood stabiliser. If they are hyper-vigilant, one of the core features of PTSD, if this spills over into paranoia will give them an anti-psychotic. And of course, you have to keep taking these drugs day-in, day-out as maintenance medications for the rest of your life. None of these different classes of drugs are curing the patient. They’re not treating the base disorder – which is trauma.”
Here in the UK psychiatrists (doctors prescribing drugs), clinical psychologists (NHS trained psychoanalysts who have lots to do) and psychotherapists (talk therapists of wildly varying quality, without medical training) have long existed seemingly independently of each other.
Personal and financial resources are required to tackle one’s mental health with impact.
“Pharmaceutical MDMA is 99.8% pure and very expensive”
I’d recommend medication, psychoanalysis and psychotherapy. But as a customer myself I know it doesn’t come cheap. The experience can be arbitrary too.
“After 30 years in psychiatry, my opinion is that psychotherapy boils down to a relationship between the patient and the therapist, and an ability for the patient to talk about their pain,” claims Sessa with authority, “that’s fine for around 50% of people with trauma based disorders.”
But not nearly for all.
“A significant half, they cannot go there to talk about their pain… they will do anything but talk about that night when they were ten years old, and their grandfather came into their bedroom,” says Dr Sessa.
Many therapists are understandably not fully prepared to deal with angry, impenetrable PTSD cases with substance use disorders and co-morbidities like ADHD.
“Trauma victims drop out of therapy. We have high rates of self harm and suicide, and very high rates of addictions. There’s a 50% treatment resistance in PTSD. After detox, 70 to 90% of addicts are back on the substance again.”
Combining psychiatry and psychotherapy sounds like common sense. But it’s practically unheard of. “The therapy alongside the MDMA makes the difference,” says Sessa pointing out that his clinic Awakn doesn’t offer its current ketamine programme without accompanying talk sessions.
Awakn conducted its BIMA – Bristol Imperial MDMA for Alcoholism – project under research trial conditions, so while the process mirrored a regular treatment programme with genuine sufferers they didn’t pay and regulations were fiercely adhered to. Pharmaceutical MDMA was used, “it’s 99.8% pure and very expensive,” says Sessa.
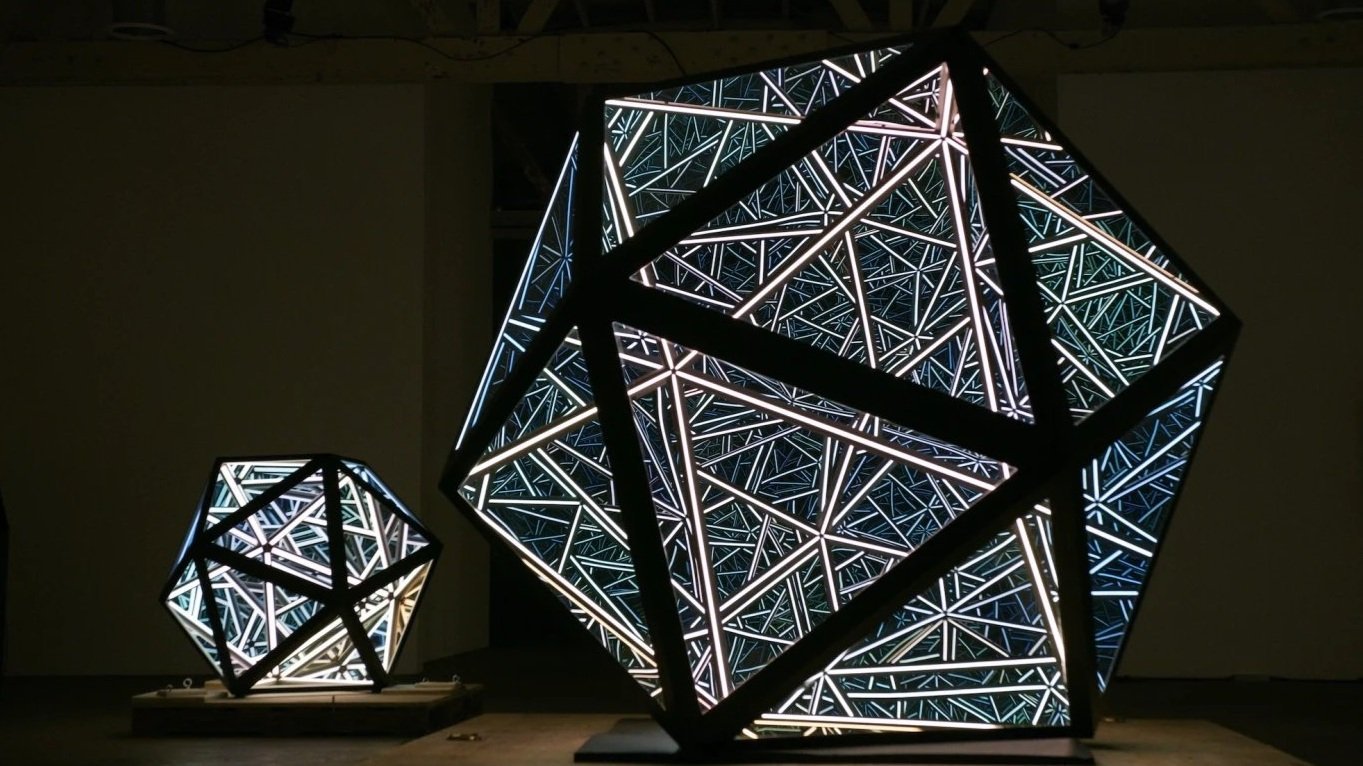
MDMA’s cocktail of positive therapeutic effects include a melodic duet between the amygdala and frontal cortex, where the amygdala ‘fear response’ shrinks while activity in the advanced brain grows, providing an ‘optimal window of arousal’. MDMA’s empathy-increasing properties, generated by production of the hormone oxytocin, strengthen the bond between therapist and patent.
“Elements of transpersonal psychotherapy were used during the drug sessions”
The ‘peak experience’ though remains key for softening the calloused neural pathways that dictate repeated cycles of dysfunctional behaviour, like addiction in particular.
“You can’t just tell someone ‘stop thinking like that’. Chronic unremitting mental disorder is all about ‘stuckness’. It becomes your version of yourself.” Decades on from the original trauma, “Something otherwise relatively benign happens in the queue at the post office and you have a panic attack,” illustrates Sessa.
BIMA’s eight-week course Sessa describes with characteristic honesty as, “‘MDMA assisted psychotherapy for the treatment of alcohol use disorder’, which is perfectly accurate. It’s never been done before; we were making it up as we went along.”
For MAPS-trained Sessa and his prodigal collaborator Dr Celia Morgan (named by Business Insider as one of the ‘Women Shaping the Future of Psychedelics’) this meant drawing on their wealth of experience carving out the Psychedelic Renaissance over the past 20 years, rather than riffing.
“Of course it was more nuanced than that. We had elements of transpersonal psychotherapy we used during the drug sessions; we used a lot taken from the maps manual for PTSD.”
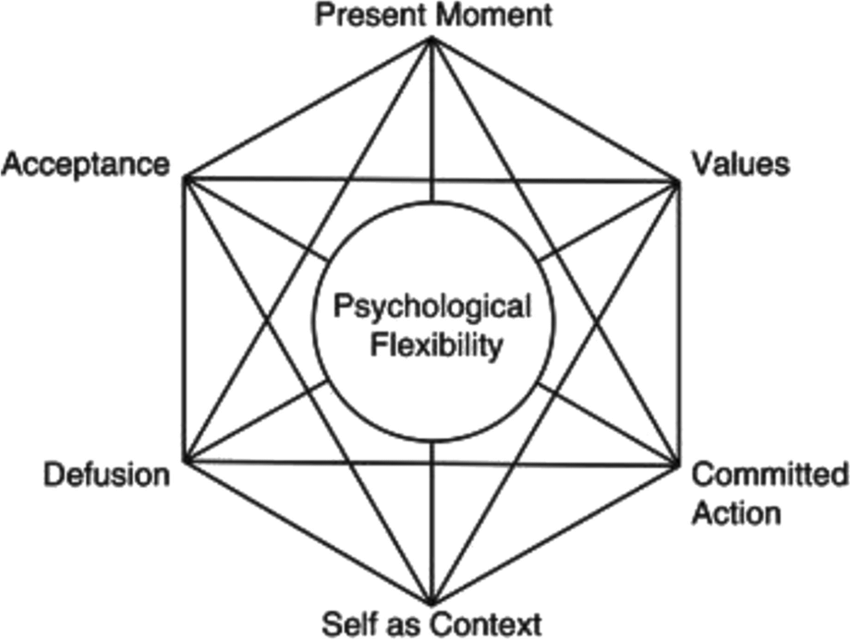
All the subjects were daily heavy drinkers who had been through detox. Talk therapy in the ‘non drug’ sessions, a total of 15 around three MDMA ‘trips’ drew from their experience at the forefront of addiction treatment: “We used elements of Acceptance and Commitment Therapy, Motivational Enhancement Therapy, and CBT [Cognitive Behavioural Therapy], which were typical for addiction studies. We are of course writing the manual for this, and will be using it as we move into Phase 2B.”