The Vine of the Soul has been synthesised. Kind of.
Pharmacusca is a combination of DMT and beta-carboline stomach inhibitor harmine, which also boasts psychedelic properties. “There’s a huge body of evidence showing ayahuasca’s therapeutic potential,” says Imperial College’s Ashleigh Murphy-Beiner who’s been a cheerleader for ayahuasca research here in the UK.
What’s used for most tests on ayahuasca, ‘The Vine of the Soul’ is ‘pharmahuasca’ a combination of DMT and harmaline, the brew’s two stand-out alkaloids, often taken as separate pills 10-20 minutes apart so the mono-inhibitors in harmine that stop the stomach from registering the fact there’s a bucket of DMT in there can take effect. Pharmahuasca’s long been gaining popularity with recreational users too.
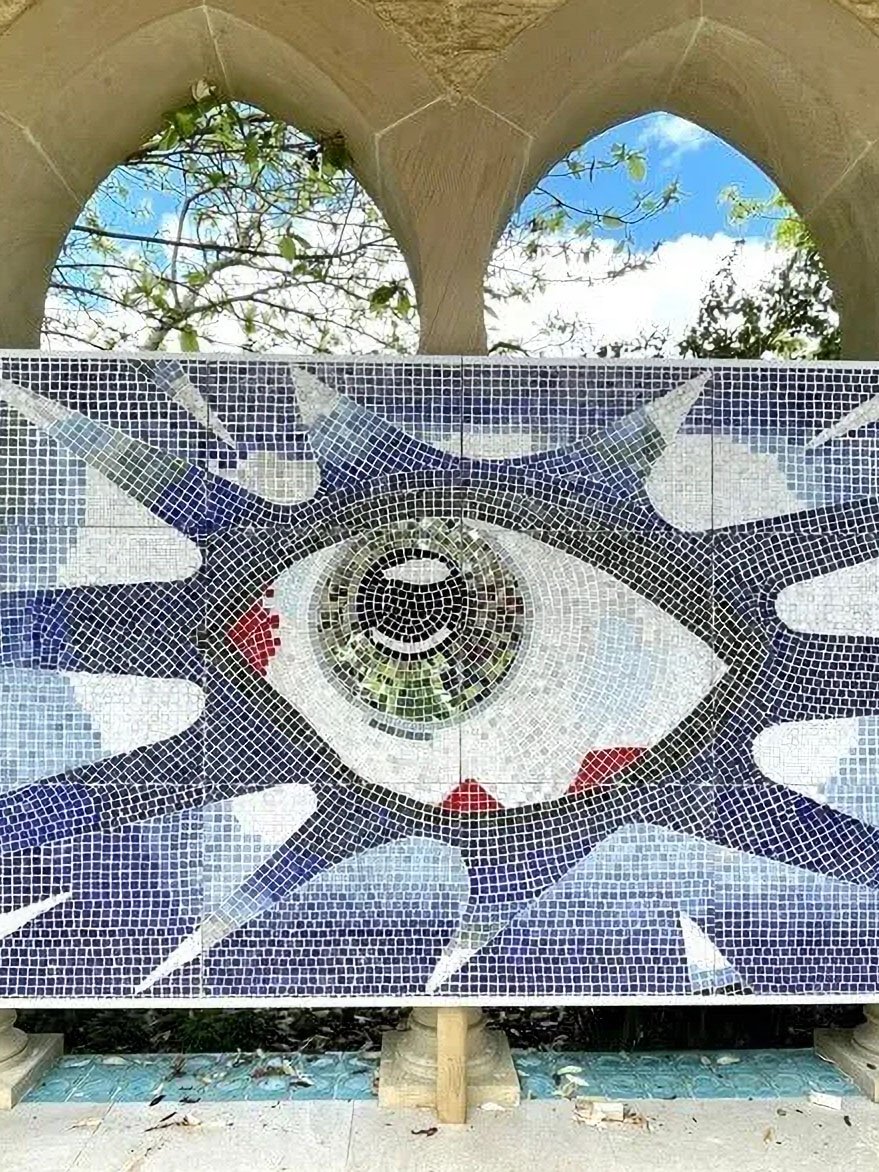
“The vines are part of a magnificent cluster of beings”
“You just use the alkaloids and you say this is equivalent,” comments Dr Luis Eduardo Luna in his lecture closing Vital’s therapy-themed teaching module examining what Western practitioners can learn from traditional amazonian approaches, “It isn’t, neither chemically or synergistically. It is reduced down to a pill… an object.”
Pharmahuasca also dispenses with the aspects of ritual, myth and ceremony – and even the digestive pruging – that are obligatory in traditional use. 2021 resarch paper Examining changes in personality following shamanic ceremonial use of ayahuasca gently insisted, ‘Ceremonial practices may be informative about key elements of psychedelic-assisted experience that potentiate positive psychological changes’ and used authentic ceremony as its laboratory setting.
Traditional ayahuasca brews contain more than two dozen active ingredients, some of which are contained in the chunky bits floating around the ichorous concoction. “The vines run throughout the forest. They are in symbiotic relationships with other plants, insects, animals and microbes, part of a magnificent cluster of beings,” says Dr Luna who cultivates an ecosystem friendly to Columbian ayahuasca equivalent yagé at his Wasiwaska nature reserve in Florentina, Brazil that you can read more about in this issue’s Integration item.
Preparations and admixtures for ayahuasca, yagé and another concoction capi differ between tribes and locations, so don’t accept any black-and-white categorisations from know it alls while debating psychedelics at one of your global north dinner parties. For example the Colombian Orinoco tribe consider ayahuasca to contain a ‘male’ spirit while it is generally thought of as ‘Mother Ayahuasca’ elsewhere and in the West.
“I believe in both approaches, science and animism. We could be epistemological polyglots”
The Colombian yagé Dr Luna first took alongside Terrence McKenna in 1971 uses the chaliponga plant as its DMT source instead of chacruna. While it may not be of relevance to Western researchers the preparation and ceremonial aspects of yagé are certainly different. Yagé’s effect is considered more contemplative and ayahuasca’s purgative, but that statement is also generalising to an inappropriate degree.
Forcing down all the ingredients ceremonially for the true effect is no piety, insists Dr Luna. Indeed traditionally ayahuasca and yagé are used to solve practical issues (for instance locating a missing cockerel, clearing out your guts) rather than ‘finding God’ as canonical maestro Maria Sabina put it.
If Westerners can come to terms with an overlap of the spiritual and the material inherent in amazonian animistic and plant medicine culture, “We could truly be epistemological polyglots – studying the living and non-living world with the precision of scientific language, while simultaneously somehow perceiving the spirit, the anima of all that exists,” said Dr Luna in his keynote speech at Exeter University Philosophy of Psychedelics conference earlier this year, titled ‘Decolonising the Self’. “I believe in both approaches, science and animism, and that they are entirely compatible in the modern world,” he edicts.
Even the paper Examining changes in personality following shamanic ceremonial use of ayahuasca printed in March 2021’s Scientific Reports slipped into the academic conversation that ‘The present study shows preliminary support for the therapeutic benefit of the shaman, icaro, purgative elements, cognitive reappraisal, sacramental atmosphere, and communal/group context.’
44% of Amazon biomass is vine. Vines are plants that require other surfaces to support themselves. They climb up these, which are mostly ‘self-supporting’ trees, using strong arterial veins pumped with water so they love rainforest. While vines might creep around and not stand up straight without leaning on something else, they’re of considerable importance to the local ecosystem and tribespeople put them to good use as a versatile building and manufacturing material. Animals use them as transport, for avoiding predators in particular. Their abandoned biomass keeps the soil below host plants nutrient rich and vines provide food and medicinal sources aplenty: grapes, cucumbers, melons, and vanilla come from vines.
Dr Luna lists the importance of ingesting the whole plant/fungus, not an extraction, in his bullet-points for Western therapists. Ideally it would be grown on-site at one’s paradisiacal retreat like Dr Luna’s Wasiwaska, a psychedelic nature reserve. Ecological projects involving the local community bring economic benefits. in the Amazon itself for example, retreats investing in the community would bring serious good vibes back in return. I’d cite Jake’s in Jamaica as a great example, would-be psychedelic travel entrepreneurs.
Ayahuasca’s shown considerable benefits to mindfulness (being ‘in the moment’) and cognitive flexibility (common sense) in tests for depression plus it’s also been a focus for studies into borderline personality and eating disorders. Leading crowdfunded research into trauma already testing DMT on rats is none other than… the esteemed Dr Robin ‘Hollywood’ Carhart-Harris, now ‘Founding Director of The Neuroscape Psychedelics Division and newly endowed Ralph Metzner Distinguished Professor of Neurology and Psychiatry at the University of California San Francisco’ (capitals all theirs). Hollywood says, ”DMT is a particularly intriguing psychedelic. The visual vividness and depth of immersion produced by high doses of the substance seems to be on a scale above what is reported with more widely studied psychedelics such as psilocybin or ‘magic mushrooms’.” Before you think ‘Isn’t that a bit of a Western science-y interpretation?’ that’s what Hollywood does – get these concepts over the line with the scientific establishment. We should thank him for that, I reckon.
Even if he is using pharmauasca. For now – because the active chemical ingredients may only play one part in the healing power of Amazonian-style plant medicine traditions. And not be so powerrful without the… is magic too strong a word? ingredients that are impossible to replicate in laboratories and treatment rooms.

























Medical, Dr Ben Sessa, Zine #14, Vital 2.6
Medical, Dr Ben Sessa, Zine #14, Vital 2.6
‘Peak early and don’t skimp on quality’ is the Awakn formula to avoid MDMA comedowns.
Medical, Dr Ben Sessa, Zine #14, Vital 2.6